Recovery After Stroke: 90-Day Timeline Doctors Focus On
A stroke can change your life in seconds, and it often leaves you and your family unsure about what recovery will truly look like. Those early days after a stroke bring fear, hope, and many questions about movement, speech, and daily independence.
Understanding how the brain heals helps you feel more prepared and less overwhelmed through each stage of recovery. Medical science now shows that early care and structured rehabilitation can make a real difference in how well a person improves.
In this blog, you will find clear, evidence-based insights on what to expect and how recovery typically unfolds in the first 90 days.
Key Takeaways:
- The first 90 days are the fastest for brain recovery due to high neuroplasticity and an early rehabilitation response.
- Timely stroke treatment improves movement, speech, and independence far more than delayed care.
- Consistent therapy and medical monitoring shape long-term recovery outcomes more than any single intervention.
Quick Answer: Most stroke recovery happens in the first 90 days, when the brain responds best to therapy, medication, and guided rehabilitation.
Quick Links
- Why the First 90 Days Matter in Recovery After Stroke
- Reasons for Stroke and Why “Heart Stroke” Is a Medical Myth
- Stroke Treatment Timeline: What Happens First and Why Early Action Matters
- What Progress Looks Like in 90 Days: Milestones Patients Notice
- Rehab Plan That Supports Recovery After Stroke
- How Doctors Track Stroke Recovery?
- Why Choose Eskag Sanjeevani for Neurological Treatments
Why the First 90 Days Matter in Recovery After Stroke
Studies point out that the initial 90 days of recovery after stroke represent the peak time for neurological healing. During this time, the brain’s neuroplasticity is at its peak and assists in targeted rehabilitation.
- Rapid Early Recovery: Studies suggest that stroke survivors achieve more than 50% functional improvement within the first two weeks after onset, with gains continuing up to 12 weeks 1.
- Critical 3-month Window: Data suggests that 48% to 91% of achievable recovery occurs within the 3-month window, making this a critical phase for rehabilitation 2.
- Therapy Time: Initiation of intensive rehabilitation within the first 60 to 90 days results in longer-term improvement than delayed therapy, especially for motor skills such as arm and hand function.
- Neuroplasticity: It is the phase in which your brain adapts and reorganises neural pathways, which is a critical element for movement, speech, and daily activities, and is strongest in the first three months after a stroke.
- Outcome Variation: While progress continues beyond 90 days, the magnitude slows after this period, and early gains strongly influence functional independence and quality of life long term.
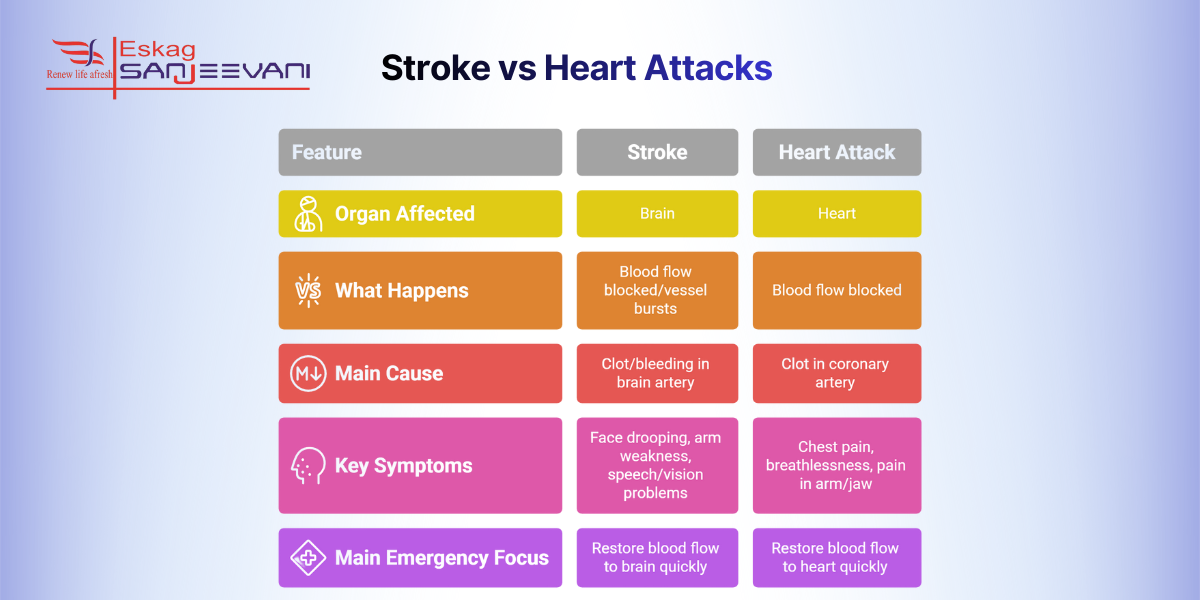
Now, with a clear understanding of the importance of the time of recovery after a stroke, let’s understand the major difference between a stroke and a heart attack.
Reasons for Stroke and Why “Heart Stroke” Is a Medical Myth
Stroke is a medical emergency, and the interruption of blood flow to the brain is the primary cause. However, heart stroke is the term most people confuse with stroke, and they think it is related to a cardiac condition. In reality, stroke and heart attack are entirely different andaffects different organs even though they share overlapping risk factors.
Understanding the reasons for stroke and how it differs from heart conditions helps clarify risks and reduce complications from a stroke later.
- Different Organs, Shared Risks: A stroke generally occurs when blood flow is restricted by a ruptured blood vessel, ultimately cutting off the oxygen supply to brain cells. A heart stroke, on the other hand, is a medical term and people use it to suggest a heart attack.
- Primary Causes of Stroke: According to the National Heart, Lung, and Blood Institute, 87% of strokes are ischemic, which majorly occurs when a clot blocks a brain artery; however rest are hemorrhagic 3. High blood pressure, diabetes, cholesterol, and irregular heart rhythms (like atrial fibrillation) are common contributing factors. High blood pressure alone accounts for up to 35-50 % of stroke risk.
- Role of arterial blockages: Plaque buildup (atherosclerosis) can occur in both the heart and brain vessels. Such blockages trigger ischemic stroke within your brain. However, similar blockages cause heart attacks, which sometimes create confusion between the two conditions.
- Transient ischemic attacks (TIAs): Commonly known as a mini stroke, a TIA occurs when there is a temporary blockage of blood within the brain and resolves in a few minutes. There are several shared causes for TIA, which signal a major stroke that may occur in the future.
Leading neurology services provide rapid triage, imaging, and clot therapy, dramatically reducing brain injury and speeding recovery.
Stroke Treatment Timeline: What Happens First and Why Early Action Matters
Stroke treatment begins with rapid assessment and intervention because recovery after stroke depends on how quickly blood flow is restored and secondary brain damage is limited. Early action within the first few hours can dramatically reduce long-term disability and improve outcomes.
Here’s a comprehensive understanding to increase the chances of meaningful recovery for a stroke patient:
- Immediate emergency response: At the first sign of stroke, rapid evaluation is the first step, including neurological exam and vital signs, often within minutes of hospital arrival. Moreover, prompt assessment accelerates decision-making and enhances overall outcomes.
- Urgent brain imaging: A CT scan or MRI determines the type of stroke, whether ischemic or hemorrhagic. Imaging is usually performed within the first hour of arrival.
- Clot-busting therapy: For ischemic strokes, intravenous thrombolysis (e.g., tPA) is most effective when given within 4.5 hours of symptom onset 4. The process can restore blood flow and reduce long-term disability.
- Endovascular procedures: In suitable cases, mechanical thrombectomy, which is physically removing a clot through a catheter, is performed after 24 hours, especially for large vessel occlusions. It extends the window for recovery potential in selected patients.
- Stabilisation and monitoring: After initial intervention, patients are monitored in a stroke unit or ICU to control blood pressure, sugar levels, and prevent complications such as swelling, bleeding, or recurrent stroke.
Also read: Critical Hours in ICU: A Step-by-Step Survival Guide for Families.
What Progress Looks Like in 90 Days: Milestones Patients Notice
For recovery after stroke, the first 90 days mark the most active phase of brain repair. Progress during this window also highlights how risk control addresses the original reasons for stroke, such as blood pressure and heart rhythm disorders.
Movement and Physical Function
Most patients show improved muscle strength and balance within the first four to six weeks after a stroke. By three months, many regain basic walking or assisted mobility, especially with early and regular physiotherapy.
Daily Independence and Cognitive Skills
Tasks such as dressing, eating, and basic hygiene often become easier as occupational therapy builds coordinated motor control. Attention and memory frequently improve during this period as the brain restores disrupted neural networks.
Speech, Swallowing, and Communication
Speech clarity and swallowing often improve during the first eight to twelve weeks due to targeted speech therapy. Neural rewiring allows language areas to adapt, so many patients notice fewer word-finding and articulation problems.
Here’s a tabular representation for an easy understanding of the timeline:
| Time Period | Typical Recovery Focus |
| First 24–72 hours | Brain protection, clot control |
| Weeks 1–4 | Rapid neurological gains |
| Weeks 5–12 | Strength, speech, independence |
| After 3 months | Slower but steady improvement |
Your neurologist guides a personalised rehab plan, so you know which therapies suit your recovery and daily goals.
Rehab Plan That Supports Recovery After Stroke
A tailored rehab plan helps gain strength for regular activities and reduce the chances of long-term disability.
Here is a detailed plan that can support an individual who is recovering from a stroke:
- Physical Therapy: Appropriate focus on strength with coordination to regain mobility and reduce the risk of falls. Better muscle control also enhances the likelihood of walking independently.
- Occupational Therapy: Helps patients resume day-to-day activities such as eating and bathing, which are often personalised.
- Emotional Support: Therapists focus on memory and problem-solving capabilities to improve quality of life.
- Medical Follow-ups: Regular reviews with your care team help adjust therapy plans and prevent the chances of recurrence and complications.
Now, with a better understanding of stroke rehabilitation, let’s explore how doctors track overall stroke recovery.
How Doctors Track Stroke Recovery?
Doctors track and support recovery after stroke by using structured assessments and personalised therapy goals throughout rehabilitation. They are also responsible for measuring improvements in movement, speech, balance and daily tasks to adjust treatment plans as needed, which helps maximise functional gains and prevent setbacks. Consistent monitoring also includes evaluating endurance and safety for activities, so clinicians can recommend the right intensity and type of support at each stage of recovery.
Why Choose Eskag Sanjeevani for Neurological Treatments
Eskag Sanjeevani hospitals operate with advanced neuro-diagnostic platforms, integrated emergency pathways, and protocol-driven critical care to manage complex cerebrovascular cases. The Dept of Neurology delivers evidence-based stroke and neuro-rehabilitation through multidisciplinary coordination among neurologists, radiologists, and intensivists. Standardised clinical pathways, round-the-clock neuro-monitoring, and outcome-tracked rehabilitation ensure precise, data-guided care from acute intervention through recovery.
Final Thoughts
Every recovery journey is different, but steady progress is far more likely when you follow a structured medical and rehabilitation plan. Make sure you attend every therapy session, take prescribed medicines regularly, and track even small improvements in daily abilities. Do not hesitate to ask your care team about new symptoms, fatigue, or emotional changes, as early support prevents long-term setbacks.
With patience and guided care, recovery after a stroke can continue well beyond the first few months with meaningful gains in independence. Support from experienced medical staff at Eskag Sanjeevani can help you stay on the right path through each stage of healing.
References
High-impact or unsupervised activities should be avoided early, especially without medical clearance. Safe activities like walking or chair-based exercises are usually encouraged under a physiotherapist’s guidance.
Recovery varies by stroke type and severity, but most neurological improvement occurs within the first three to six months. However, long-term gains can continue for years with structured rehabilitation guided by neurologists and physiotherapists.
Worsening weakness, new speech problems, severe headache, or reduced consciousness require immediate medical review as they may signal brain swelling or another stroke. Persistent fever, chest pain, or difficulty breathing also need urgent evaluation to prevent serious complications.
Preventing a second stroke requires strict adherence to prescribed medications such as antiplatelets, blood pressure drugs, and cholesterol control. Lifestyle changes and regular follow-ups with a neurologist significantly reduce recurrence risk.
ICU stay varies based on stroke severity and complications, often lasting 24 hours to several days. Some patients require longer monitoring before shifting to rehabilitation units.

