Pneumonia in Children: Symptoms, Risks, and When to Seek Care
Pneumonia in children remains a serious respiratory condition that can progress rapidly without early attention and timely care. In India, pneumonia accounts for nearly 14% of deaths among children under five, highlighting its public health impact 1.
Seeing a child struggle with a fever, cough, or breathing can feel frightening and overwhelming for any parent. Explicit knowledge helps parents respond calmly and seek care at the right time.
In this blog, we explain pneumonia in children, the symptoms to watch, and when medical help becomes essential.
Key Takeaways:
- Pneumonia in children can progress promptly, making early symptom recognition essential for timely medical care.
- Breathing difficulty, fever, and low energy are key warning signs that need close attention.
- Pneumonia can spread through close contact, but simple hygiene measures can reduce the risk of infection.
3 Primary Types of Pneumonia
Pneumonia is an inflammation of the lungs caused by bacteria, chemical irritants, and viruses. It is a significant infection which fills alveoli with pus and other liquids and is life-threatening for children.
Here are some of the significant types of pneumonia:
- Bacterial pneumonia: Streptococcus pneumoniae is the primary cause. May other bacteria cause infections and symptoms include fatigue, fever, chest pain, and more.
- Viral pneumonia: Respiratory syncytial virus (RSV), parainfluenza virus, and adenovirus are among the viruses responsible for the condition.
- Mycoplasma pneumonia: The condition causes mild symptoms such as fever and cough. This is also known as walking pneumonia, as patients are highly active and the infection is not severe.
Understanding pneumonia in children begins with noticing subtle early symptoms at home.
Symptoms of Pneumonia in Children: Early Signs Parents Notice
Pneumonia in children often begins with subtle symptoms that may resemble a common cold but worsen rapidly. Early recognition of these signs helps parents seek timely care before breathing difficulties increase.
Here are some of the symptoms of pneumonia in children:
- Persistent fever: A high or recurring fever that does not settle with routine care can indicate an underlying lung infection.
- Fast or laboured breathing: Accelerated breathing, flaring of the nostrils, or visible chest movement suggest the lungs are struggling to supply enough oxygen
- Continuous cough: A cough that becomes deeper, more frequent, or more painful may signal lung inflammation.
- Unusual tiredness or reduced activity: Signs of weakness or reluctance to play among children due to reduced oxygen levels.
- Poor feeding or appetite loss: Infants and young children often feed less or refuse food when breathing becomes uncomfortable.
Pneumonia in children often alters breathing patterns and significantly depletes energy early.
How Pneumonia Affects a Child’s Breathing and Energy Levels
Pneumonia in children often leads to low oxygen levels and rapid breathing because the lungs become filled with fluid and inflammatory cells rather than air. Research suggests that about 35.9 % of children hospitalised with pneumonia develop hypoxia 2.
Such respiratory changes directly affect children’s energy levels and make simple activities more stressful.
- Rapid respiratory rate: When air sacs fill with fluid, children breathe faster, like in chronic obstructive pulmonary disorders (COPD), tiring their respiratory muscles quickly.
- Lowered oxygen saturation: Hypoxia, a condition often associated with pneumonia, reduces oxygen availability in the alveoli and restricts overall airflow. It ultimately leads to a lack of physical activity.
- Reduced feeding and play: When oxygen demand increases, a child may refuse food and avoid play. Such a reduction is generally for energy conservation, which is an involuntary condition during pneumonia.
- Chest retractions: Visible pulling in of the chest wall with each breath indicates increased work of breathing and poor lung expansion, which can add to fatigue.
- Lowered oxygen saturation: Hypoxia reduces oxygen delivery to vital organs and muscles, leading to lethargy and reduced tolerance to physical activity in affected children.
A proper understanding of spread helps guide timely pneumonia medication and protect children from infection.
Is Pneumonia Contagious? How It Spreads and How to Reduce Risk
Pneumonia in children can be contagious when caused by bacteria or viruses, especially in shared indoor environments. Transmission risk increases when close contact, poor ventilation, or weakened immunity is present.
Here are some of the factors to understand why is pneumonia contagious among children:
- Respiratory droplet spread: Coughing, sneezing, or conversations in proximity release infected droplets that can enter another child’s airways.
- Household and school exposure: Classrooms and community gatherings are hotspots for communicable diseases. Disease transmission is prevalent in areas with large populations.
- Post-viral vulnerability: Children with pre-existing respiratory disease experience delayed recovery because the nasal airway lacks the necessary defences against bacterial infections.
Indirect contact through surfaces: Germs on toys, door handles, or utensils can be transmitted when children touch their face or mouth.
Practical prevention steps: Hand hygiene, respiratory etiquette, clean surroundings, vaccinations, and early isolation reduce the volatility of the disease and limit transmission.
Also read: Winter Pneumonia Risks Explained
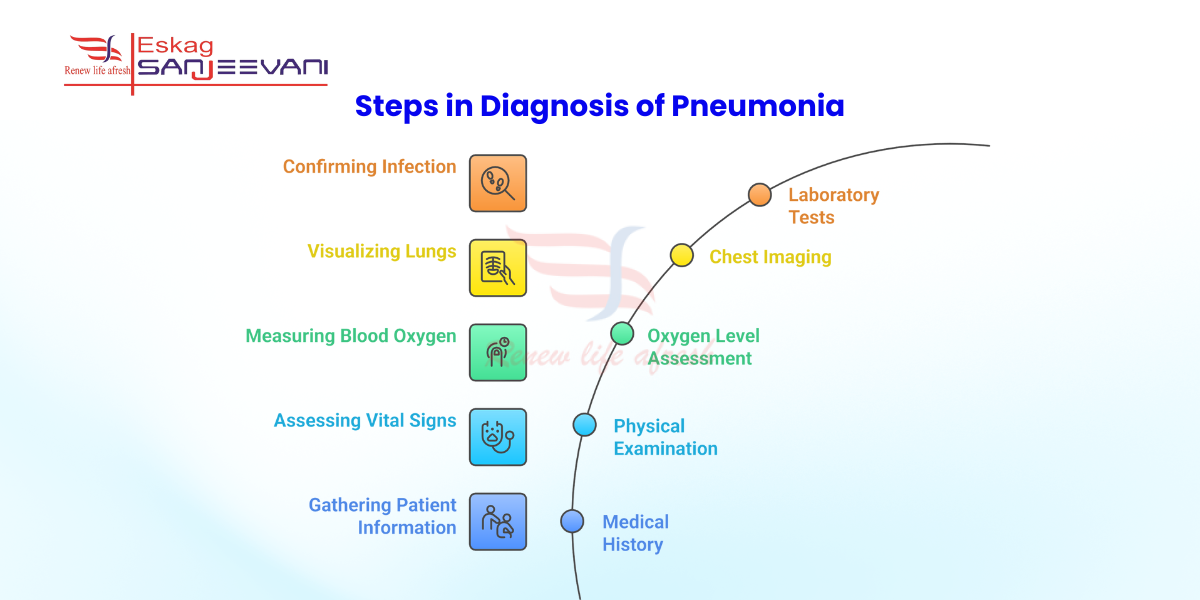
How Doctors Diagnose Pneumonia in Children
Doctors diagnose pneumonia in children through a careful combination of clinical assessment and targeted tests, based on the child’s age, symptoms, and severity.
- Detailed medical history: Doctors ask about the duration of fever, cough pattern, breathing difficulty, feeding behaviour, and recent infections or exposures.
- Physical examination: Chest examination is vital for identifying signs of rapid breathing, chest indrawing, reduced air entry, or abnormal lung sounds that suggest infection.
- Oxygen level assessment: Pulse oximetry is a critical technique for measuring blood oxygen saturation levels to identify hypoxia, which is a severe case of pneumonia.
- Chest imaging: A chest X-ray is a necessary diagnostic test to assess symptom severity and identify lung involvement or complications.
- Laboratory tests: Blood tests or microbiological samples may help identify bacterial infection or pulmonary fibrosis, especially in hospitalised children.
Final Thoughts
Pneumonia in children deteriorates in a fast-fashion, and early recognition of breathing changes, energy loss, and feeding difficulties becomes difficult to isolate by healthcare professionals. A timeline from medical professionals helps reduce further complications and quick recovery, especially among young individuals with critical conditions. Moreover, it is necessary to know the symptoms along with the diagnosis, so parents can monitor the condition and ensure prompt treatment.
At Eskag Sanjeevani Hospital, children receive structured respiratory care supported by experienced pulmonologists in Kolkata and child-focused diagnostic services. A proactive, stepwise approach ensures an appropriate diagnosis for pneumonia treatment and close monitoring when needed. Seeking expert care early can protect lung health and reduce long-term risks for growing children.
References
The overall severity of pneumonia among children can range from mild to life-threatening conditions. The progression of the condition depends on age and cause; early interventions are necessary to prevent disease severity.
A cough associated with pneumonia improves with proper medical treatment and adequate rest. Keeping the child hydrated and following the doctor’s advice helps relieve symptoms.
In most cases, children recover from instances of excruciating pneumonia with appropriate diagnosis and medication. Children without any comorbidities or pre-existing conditions often recover quickly from the disease.
Recovery time for mild cases often ranges from 1 to 3 weeks. Severe pneumonia may require longer follow-up and monitoring.
Prompt medical intervention, along with proper diet, is a prerequisite for a pneumonia treatment plan. Moreover, regular monitoring is critical to avoid strains and support recovery plans to maintain lung health

