Cold and Chest Infection: Key Symptoms and Treatments Explained
Common colds are now widespread, and with cold wave conditions prevalent in India, they are a critical issue in most households. Respiratory infections cause a whopping 3,740 deaths across India, which contributes to the 18% of the global population 1. It is essential to look for early warning signs and symptom patterns which help determine the extent of such respiratory conditions.
In this blog, we will explore the key differences between the common cold and chest infections, along with treatments that can help relieve these conditions.
Key Takeaways:
- A chest infection affects the lungs and causes more severe symptoms, while a common cold affects the upper airways and is usually mild.
- Cold symptoms often resolve with home care, but chest infection symptoms may require medical evaluation.
- Early consultation at a hospital helps prevent complications and ensures proper respiratory treatment.
Quick Links

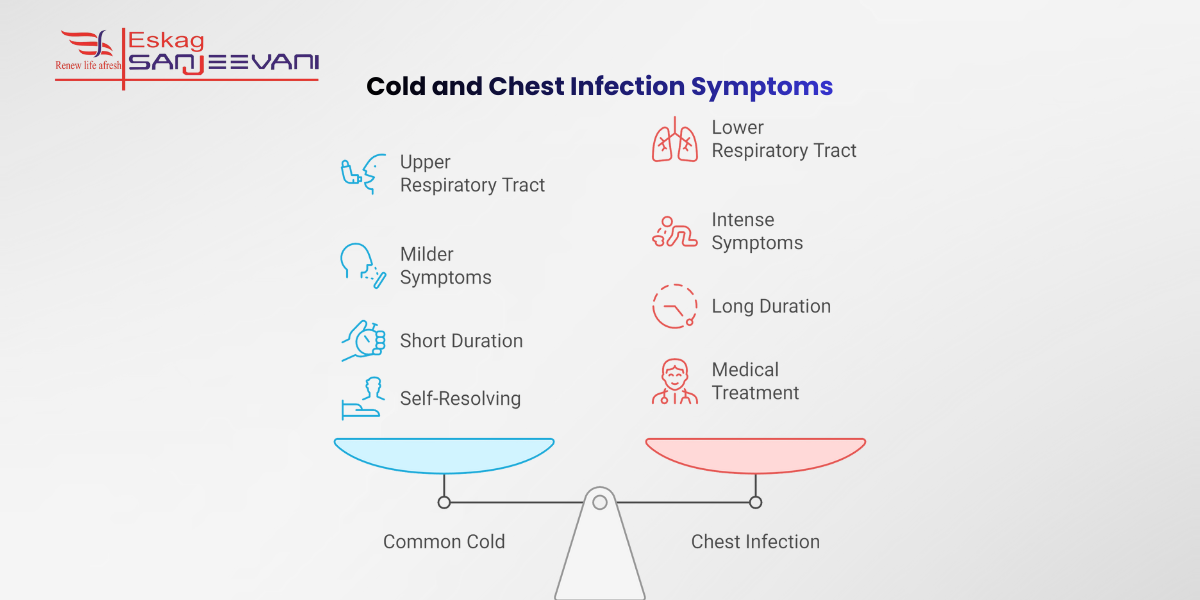
What Is the Difference Between a Cold and a Chest Infection?
Cold and chest infections are both types of respiratory illnesses, but they affect different parts of the respiratory system and vary in severity. In India, acute respiratory infections (ARIs), with colds and chest infections, affect about 2.79% of children nationwide 2.
Here are some of the major differences you must know between the two conditions:
- A common cold is an infection of the upper respiratory tract, primarily the nose, sinuses and throat. Viruses usually cause it, and it often resolves on its own.
- A chest infection impacts the lower respiratory tract, including the airways and lungs. It can include conditions like bronchitis and pneumonia.
- With a cold, symptoms are generally milder, for example, a runny or blocked nose and sneezing.
- Chest infections and asthma tend to cause more intense symptoms, such as a productive cough with coloured mucus, chest discomfort and breathlessness.
- While a cold often resolves within 7 to 10 days, a chest infection may require medical assessment and treatment, especially if symptoms are severe or persistent.
Let’s now explore some common cold symptoms that help determine the causes of the common cold and guide accurate interventions.
Common Cold Symptoms: What to Expect
The common cold usually starts with mild symptoms affecting the upper respiratory system and typically develops 1–3 days after exposure to a cold virus. Most people recover within about 7–10 days, though some symptoms may linger slightly longer.
Here’s a detailed look at what to expect with a common cold:
- Runny or stuffy nose: You may start with clear nasal discharge that can thicken and change colour over time; this does not automatically mean a bacterial infection. Many people also feel their nose becoming blocked or congested, making breathing through the nose harder.
- Sore or scratchy throat: Early in the illness, you may notice irritation or soreness at the back of the throat, which can make swallowing uncomfortable or irritating until the body fights off the virus.
- Sneezing and cold fever: Sneezing is common, and most individuals feel unwell or experience a slight cold fever. However, high fever is uncommon in such cases.
- Low‑grade fever: A negligible increase in body temperature may occur, especially in children, but a significantly high fever is not typical of a simple cold.
- Cough and cold cough: A cold cough often develops as the cold progresses and can range from dry to more persistent, though it usually remains milder than coughs seen with chest infections.
Next, let’s explore some of the critical chest infection symptoms that lead to long-term chronic chest conditions.
Key Symptoms of a Chest Infection
A chest infection refers to a disease of the airways or lungs and can be more serious than a common cold, especially if symptoms persist or worsen. Acute bronchitis is one of the common cold and chest infection affects 5% of global adults, which makes respiratory conditions like cold cough critical 3.
- Cough with or without phlegm: A cough that stays for days, often producing thick mucous, can be a key sign of a chest infection and bronchitis rather than a simple cold. This cough may disrupt sleep and daily activities.
- Fast breathing: You may breathe quicker than usual or feel short of breath, which can signal inflammation of the airways or lungs.
- Chest pain: Pain or excessive pressure in the chest, when breathing deeply or coughing, can indicate irritation of the chest wall or lungs. The discomfort may continue until the inflammation subsides.
- Fever: A high temperature (fever) often accompanies cold and chest infections as your body fights the disease, and you may feel unusually fatigued or worn out.
- Faster heart rate: Your heart may beat faster than usual during a chest infection as your body responds to infection and increased breathing effort. It can contribute to a sense of overall discomfort.
Also read: All You Need To Know About Winter Lung Care
Treatment for Cold vs Chest Infection: What You Need to Know
When it comes to cold and chest Infection treatment and managing similar respiratory illnesses, such as a common cold, understanding the difference in approach is key.
A cold usually needs simple supportive care, while a chest infection often requires a more targeted plan, depending on whether it’s viral or bacterial.
Treatment for Viral Chest Infections
Most chest infections, those that start with a cold, originate from viruses and do not require antibiotics. Supportive interventions such as rest, fluids, and warm steam inhalation can ease symptoms. In more severe viral cases, doctors may consider antiviral medications to help shorten the illness.
Treatment for Bacterial Chest Infections
When a bacterial infection is diagnosed, chest infection treatment typically includes prescribed medications to neutralise the bacteria. Additionally, anti‑inflammatory drugs and fever-reducing medications help manage discomfort and accelerate recovery. Some patients may also benefit from nebulisation therapy to open airways and improve breathing.
Hospital and Advanced Care for Severe Cases
If a chest infection becomes serious, hospital care is necessary, with oxygen therapy and close monitoring. In such situations, consulting the best pulmonologists in Kolkata ensures precise treatment tailored to your condition.
When Should You See a Chest Specialist?
If you experience symptoms such as a cough, shortness of breath, or wheezing, it’s important to consult a chest specialist at Eskag Sanjeevani hospitals. Symptoms lasting more than 3 weeks, including chest pain, fever, or difficulty breathing, may indicate a serious condition that requires professional attention.
If you’re coughing up blood or thick mucus or experiencing severe breathing difficulties, immediate evaluation by a pulmonologist is necessary. Additionally, individuals with pre‑existing lung conditions like asthma or COPD should regularly consult a chest specialist to manage their health effectively and prevent complications.
Final Thoughts
Cold and chest infection often appear similar, but early symptom awareness helps you choose timely care and prevent complications. Most colds settle with rest, while chest infections may need medical evaluation, especially if breathing symptoms worsen or persist. If symptoms escalate, prompt consultation at a hospital ensures accurate diagnosis, appropriate treatment, and safer recovery.
References
Yes, a chest infection can develop after a cold if the infection spreads from the upper airways to the lungs. This is more likely when immunity is low, symptoms persist, or proper rest and care are delayed.
The fastest recovery depends on the cause; viral infections need rest, fluids, and symptom relief, while bacterial infections require prescribed antibiotics. Early medical evaluation ensures the correct treatment and prevents complications.
Warm soups, citrus fruits, garlic, ginger, turmeric, and protein-rich foods support immune response and help loosen mucus. Staying well hydrated also aids recovery by keeping airways clear.
There is no instant cure, but adequate sleep, warm fluids, steam inhalation, and rest can ease symptoms and support recovery. Over-the-counter medicines may reduce discomfort, but do not shorten the illness.
Balanced nutrition, regular sleep, stress control, physical activity, and good hygiene strengthen immunity over time. Adequate intake of vitamin C, vitamin D, zinc, and protein also supports respiratory defence.

